How common is diabetes in the US?
According to the CDC, 1 in 10 Americans have diabetes, 90-95% of this is Type 2 and 1 in 5 don’t know they have it. Type 2 diabetes most often develops in people over age 45, but more and more children, teens, and young adults are also developing it.
Diabetes is the 7th leading cause of death in the US, it is the number 1 cause of kidney failure, lower-limb amputations and adult blindness.
In the last 20 years, the number of adults diagnosed with diabetes has more than doubled.
There are 3 main types of diabetes
Type 1
Type 2
Gestational Diabetes
Prediabetes
According to the CDC, in the US more than 1 in 3 Americans have prediabetes, 8 in 10 of them don’t know they have it. Prediabetes raises your risk of Type 2 diabetes, heart disease and stroke.
Most of the glucose in your body comes from the food you eat. When food is digested, sugar enters your bloodstream. Insulin allows sugar to enter your cells (it is like a key to open the lock on your cells) — and lowers the amount of sugar in your blood.
Insulin is produced by a gland located behind the stomach called the pancreas. Your pancreas sends insulin to your blood when you eat. When your blood sugar level starts to drop, the pancreas slows down the secretion of insulin into the blood.
When you have prediabetes, this process doesn’t work as well. As a result, instead of fueling your cells, sugar builds up in your bloodstream. This can happen because:
- Your pancreas may not make enough insulin
- Your cells become resistant to insulin and don’t allow as much sugar in
Progression from prediabetes to type 2 diabetes isn’t inevitable.
The exact cause of prediabetes is unknown; however, family history and genetics does play a part.
There are several risk factors for prediabetes:
Overweight
Waist size
Diet
Inactivity
Age
Family history of type 2 diabetes
Gestational diabetes
Polycystic ovary syndrome
Sleep
High blood pressure
Low HDL
High triglycerides
Smoking
The more fatty tissue you have — especially inside and between the muscle and skin around your abdomen — the more resistant your cells become to insulin. Eating red and/or processed meat and drinking sugar-sweetened beverages is associated with a higher risk of prediabetes.
Although diabetes can develop at any age, the risk of prediabetes increases after age 45.
People with obstructive sleep apnea — a condition that disrupts sleep repeatedly — have an increased risk of insulin resistance. People who are overweight or obese have a higher risk of developing obstructive sleep apnea.
Prevention of prediabetes:
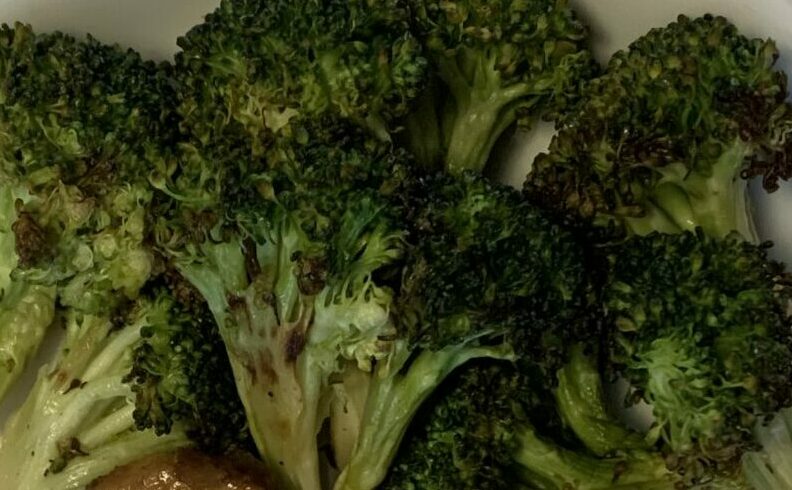
Eat healthy foods (vegetables, fruits, whole grains, lean proteins, nuts, seeds, pulses)
Get active (minimum 150 minutes of moderate physical activity per week)
Lose excess weight (5-7%)
Control blood pressure and cholesterol
Complications of prediabetes:
Long-term damage to heart, blood vessels and kidneys, even if you haven’t progressed to type 2 diabetes.
Diagnosing prediabetes
Glycated hemoglobin A1C test: average blood sugar over 2-3 months
Below 5.7% is normal
Between 5.7 and 6.4 is prediabetes
6.5% or higher on 2 separate tests indicates diabetes
Fasting blood sugar test:
Blood sample taken after not eating for at least 8 hours
Normal: less than 100
Prediabetes 100-125
The American Diabetes Association (ADA) recommends that diabetes screening for most adults begin at age 45. The ADA advises diabetes screening before age 45 if you’re overweight and have additional risk factors for prediabetes or type 2 diabetes.
Treatment for prediabetes
Eat healthy foods (vegetables, fruits, whole grains, lean proteins, nuts, seeds, pulses)
Be more active (minimum of 150 minutes of moderate physical activity per week)
Lose excess weight (5-7%)
Stop smoking
Take medications as needed
Type 1 Diabetes
The exact cause is unknown. It is thought to be an autoimmune issue, where the body destroys the islet cells that produce insulin in the pancreas. Other possible causes include genetics, exposure to viruses and other environmental factors.
Although type 1 diabetes usually appears during childhood or adolescence, it can develop in adults.
Even after a lot of research, type 1 diabetes has no cure. Treatment is directed toward managing the amount of sugar in the blood using insulin, and diet and lifestyle to prevent complications.
The role of insulin
The pancreas puts insulin in the bloodstream, insulin travels through the body allowing sugar to enter the cells, insulin lowers the amount of sugar in the bloodstream. As blood sugar drops the pancreas puts less insulin in the bloodstream. Once a large number of islet cells are destroyed, the body will produce little or no insulin. Insulin is a hormone that comes from a gland behind and below the stomach (pancreas).
The role of glucose
Glucose comes from two major sources: food and the liver
Sugar is absorbed in the bloodstream, where it enters cells with the help of insulin. The liver stores glucose in the form of glycogen. When glucose levels are low, such as when you haven’t eaten in a while, the liver breaks down the stored glycogen to glucose. This keeps glucose levels within a typical range.
Glucose — a sugar — is a main source of energy for the cells that make up muscles and other tissues.
In type 1 diabetes, there’s no insulin to let glucose into the cells. Because of this, sugar builds up in the bloodstream. This can cause life-threatening complications such as diabetic ketoacidosis.
Risk factors for Type 1
Family history
Genetics
Geography
Age
Prevention:
There is no way to prevent Type 1 diabetes
The number of people who have type 1 diabetes tends to be higher as you travel away from the equator. Anyone with a parent or sibling with type 1 diabetes has a slightly higher risk of developing the condition. Type 1 diabetes can appear at any age, but it appears at two noticeable peaks. The first peak occurs in children between 4 and 7 years old. The second is in children between 10 and 14 years old.
Researchers are working on preventing the disease or further damage of the islet cells in people who are newly diagnosed.
Complications of Type 1
Heart and blood vessel disease
Nerve damage (neuropathy)
Kidney damage (nephropathy)
Eye damage
Foot damage
Skin and mouth conditions
Pregnancy complications
Diagnosis of Type 1
Glycated hemoglobin A1C
Fasting blood sugar test
Random blood sugar test
C-peptide (measures amount of insulin produced) simultaneously with fasting glucose (this helps distinguish between type 1 and type 2)
Treatment of Type 1
Insulin (short acting, rapid acting, intermediate, long and ultra-long acting)
Count carbs, fats and proteins
Monitor blood sugar often
Eat healthy foods (vegetables, fruits, nuts, seeds, whole grains, pulses)
Exercise regularly and keep a healthy weight (minimum of 150 minutes of moderate physical activity per week)
The goal is to keep the blood sugar level as close to normal as possible to delay or prevent complications. Generally, the goal is to keep the daytime blood sugar levels before meals between 80 and 130 mg/dL (4.44 to 7.2 mmol/L). After-meal numbers should be no higher than 180 mg/dL (10 mmol/L) two hours after eating.
Gestational Diabetes
During pregnancy, your body goes through changes such as making more hormones and weight gain. These changes cause your body to use insulin less effectively, which is insulin resistance. All pregnant women have some insulin resistance during late pregnancy. However, some have insulin resistance before pregnancy. They start their pregnancy with increased need for insulin and are more likely to have gestational diabetes.
It’s important to be tested for gestational diabetes so you can begin treatment to protect your health and your baby’s health. Gestational diabetes usually develops around the 24th week of pregnancy, so you’ll probably be tested between 24 and 28 weeks.
If you’re at higher risk for gestational diabetes, your doctor may test you earlier. Blood sugar that’s higher than normal early in your pregnancy may indicate you have type 1 or type 2 diabetes rather than gestational diabetes.
Prevention
Before you get pregnant, you may be able to prevent gestational diabetes by losing weight if you’re overweight and getting regular physical activity.
Don’t try to lose weight if you’re already pregnant. You’ll need to gain some weight—but not too quickly—for your baby to be healthy. Talk to your doctor about how much weight you should gain for a healthy pregnancy.
Type 2 diabetes
With Type 2 diabetes there are two interrelated problems at work:
- Your pancreas does not produce enough insulin
- Cells respond poorly to insulin and take in less sugar
Why this happens is unknown but being overweight and inactive are contributing factors.
Type 2 diabetes used to be known as adult onset, but the increase in childhood obesity has also increased the number of cases of Type 2 in younger people.
If you have type 2 diabetes, cells don’t respond normally to insulin; this is called insulin resistance. Your pancreas makes more insulin to try to get cells to respond. Eventually your pancreas can’t keep up, and your blood sugar rises, setting the stage for prediabetes and type 2 diabetes
Type 2 diabetes symptoms
Increased thirst
Frequent urination
Increased hunger
Unintended weight loss
Fatigue
Blurred vision
Slow healing sores
Frequent infections
Numbness or tingling and hands or feet
Areas of darkened skin usually in the armpits and neck
Type 2 diabetes risk factors
Weight (overweight or obese)
Weight distribution (abdominal body fat)
Inactivity
Family history of Type 2
Race and ethnicity
Blood lipid levels
Age
Prediabetes
History of gestational diabetes
Polycystic ovary syndrome
Darkened skin around armpits and neck
Storing fat mainly in your abdomen — rather than your hips and thighs — indicates a greater risk. Your risk of type 2 diabetes rises if you’re a man with a waist circumference above 40 inches (101.6 centimeters) or a woman with a measurement above 35 inches (88.9 centimeters).
Although it’s unclear why, people of certain races and ethnicities — including Black, Hispanic, Native American and Asian people, and Pacific Islanders — are more likely to develop type 2 diabetes than white people are.
An increased risk is associated with low levels of high-density lipoprotein (HDL) cholesterol — the “good” cholesterol — and high levels of triglycerides.
Type 2 diabetes complications and comorbidities
Heart and blood vessel disease
Nerve damage in limbs (neuropathy)
Other nerve damage
Kidney disease
Eye damage
Skin conditions
Slow healing
Hearing impairment
Sleep apnea
Dementia
Type 2 diabetes is associated with an increased risk of heart disease, stroke, high blood pressure and narrowing of blood vessels (atherosclerosis). High blood sugar over time can damage or destroy nerves, resulting in tingling, numbness, burning, pain or eventual loss of feeling that usually begins at the tips of the toes or fingers and gradually spreads upward. Damage to nerves of the heart can contribute to irregular heart rhythms. Nerve damage in the digestive system can cause problems with nausea, vomiting, diarrhea or constipation. For men, nerve damage may cause erectile dysfunction.
Diabetes increases the risk of serious eye diseases, such as cataracts and glaucoma, and may damage the blood vessels of the retina, potentially leading to blindness. Diabetes may leave you more susceptible to skin problems, including bacterial and fungal infections.
Type 2 diabetes seems to increase the risk of Alzheimer’s disease and other disorders that cause dementia. Poor control of blood sugar levels is linked to more-rapid decline in memory and other thinking skills.
Type 2 diabetes prevention
Eat healthy foods (vegetables, fruits, whole grains, nuts, seeds, lean proteins, pulses)
Get active (minimum of 150 minutes of moderate physical activity per week)
Lose weight (5-10%)
Avoid inactivity for long periods of time. Sitting still for long periods can increase your risk of type 2 diabetes. Try to get up every 30 minutes and move around for at least a few minutes.
Type 2 diabetes diagnosis/treatment
Glycated hemoglobin A1C
Random blood sugar test
Fasting glucose test
Oral glucose tolerance test
Treatment
Healthy eating
Regular exercise
Weight loss
Diabetes medication or insulin therapy
Blood sugar monitoring
Contrary to popular perception, there’s no specific diabetes diet. However, it’s important to center your diet around:
- A regular schedule for meals and healthy snacks
- Smaller portion sizes
- More high-fiber foods, such as fruits, non-starchy vegetables and whole grains
- Fewer refined grains, starchy vegetables and sweets
- Modest servings of low-fat dairy, low-fat meats and fish
- Healthy cooking oils, such as olive oil or canola oil
- Fewer calories
Exercise is important for losing weight or maintaining a healthy weight. It also helps with regulating blood sugar levels. Talk to your primary health care provider before starting or changing your exercise program to ensure that activities are safe for you.
Aerobic exercise. Choose an aerobic exercise that you enjoy, such as walking, swimming, biking or running. Adults should aim for 30 minutes or more of moderate aerobic exercise on most days of the week, or at least 150 minutes a week. Children should have 60 minutes of moderate to vigorous aerobic exercise daily.
Resistance exercise. Resistance exercise increases your strength, balance and ability to perform activities of daily living more easily. Resistance training includes weightlifting, yoga and calisthenics.
Adults living with type 2 diabetes should aim for two to three sessions of resistance exercise each week. Children should engage in activities that build strength and flexibility at least three days a week. This can include resistance exercises, sports and climbing on playground equipment.
Limit inactivity. Breaking up long bouts of inactivity, such as sitting at the computer, can help control blood sugar levels. Take a few minutes to stand, walk around or do some light activity every 30 minutes.
Weight loss results in better control of blood sugar levels, cholesterol, triglycerides and blood pressure. If you’re overweight, you may begin to see improvements in these factors after losing as little as 5% of your body weight. However, the more weight you lose, the greater the benefit to your health and disease management.
Type 2 diabetes medications
Metformin: usually the first medication given, lowers glucose production in the liver and improves sensitivity to insulin
Sulfonylureas: (glipizide) increases secretion of insulin
Glinides (repaglinide): stimulates pancreas to secrete more insulin, this is faster effect than glipizide drugs, with shorter acting length of time
Thiazolidinediones (actos, avandia): makes the body’s tissues more sensitive to insulin
DPP-4 inhibitors (januvia): reduce blood sugar but tend to have a modest effect.
GLP-1 receptor agonists (Ozempic): slows digestion, lowers blood sugar, aids in weight loss and may reduce risk of heart attack and stroke
SGLT2 inhibitors (Jardiance): affect the blood filtering effects of your kidneys by inhibiting the return of glucose to your bloodstream. As a result, glucose is excreted in the urine.
Type 2 diabetes and insulin
Some people with Type 2 diabetes need insulin therapy. It used to be a last resort, but today it is prescribed sooner if blood sugar targets aren’t met with lifestyle changes and other medications. With poorly controlled glucose over time the body stops being able to make enough insulin to force its way into the cells. When this happens, insulin is usually needed
Can Type 2 turn into Type 1?
No, it cannot, they are caused by different issues. Type 1 is genetic, or autoimmune where Type 2 is not. However, over time how your Type 2 medications are managed may need to change because diabetes is a progressive disease.
After your initial diagnoses of type 2 diabetes, you may notice that it’s harder to reach your diabetes treatment targets even though your medication, exercise routine, diet, or other things you do to manage your diabetes hasn’t changed—and that’s normal. Every so often, your routine to manage your diabetes will likely need to be adjusted. You might start managing your diabetes with diet and exercise alone, but, over time, will have to progress to medication, and further down the line you might need to take a combination of medications, including insulin.
How is Type 2 diabetes progressive?
First, your body stops making enough insulin or using insulin it does make properly. When your body doesn’t use insulin properly, it’s called insulin resistance. Your beta cells increase the amount of insulin they produce to make up for the insulin resistance. Over time, the body works even harder to make more insulin and eventually it can’t keep up.
Chain reaction
- The body becomes resistant to its own insulin
- Beta cells pump out more insulin to make up for insulin resistance
- Beta cells can’t keep up with insulin needs and blood sugar levels rise to levels high enough to diagnose diabetes
- Lifestyle changes (diet and exercise) and medications (oral or injectable) are used to manage blood sugar
- Your body can’t keep up with the amount of insulin needed to manage your blood sugar and more medications are needed over time
Is Type 2 diabetes reversible?
No. According to recent research, type 2 diabetes cannot be cured, but individuals can have glucose levels that return to non-diabetes range, (complete remission) or pre-diabetes glucose level (partial remission) The primary means by which people with type 2 diabetes achieve remission is by losing significant amounts of weight.
We talk of remission and not a cure because it isn’t permanent. The beta cells have been damaged and the underlying genetic factors contributing to the person’s susceptibility to diabetes remain intact. Over time the disease process reasserts itself and continued destruction of the beta cells ensues. An environmental insult such as weight gain can bring back the symptomatic glucose intolerance.
*Sources for this presentation are: mayoclinic.org, CDC.gov, Joslin.org, diabetes.org